|
Research Ideas and Outcomes :
Research Idea
|
|
Corresponding author: Dawid Gondek (dawid.gondek.14@ucl.ac.uk)
Received: 20 Mar 2021 | Published: 22 Mar 2021
© 2021 Dawid Gondek, Bettina Moltrecht, George Ploubidis
This is an open access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation:
Gondek D, Moltrecht B, Ploubidis GB (2021) Mental health crisis in midlife – a proposed research agenda. Research Ideas and Outcomes 7: e66204. https://doi.org/10.3897/rio.7.e66204
|
|
Abstract
There is a growing amount of evidence indicating increased levels of psychological distress, suicide rates and decreased well-being in midlife (age 45-55). We refer to this phenomenon as the ‘midlife mental health crisis’. As there is little empirical evidence or theoretical grounds to explain the midlife mental health crisis, we propose a research agenda.
In order to facilitate further research, we consulted members of public, mental health professionals and researchers on potential reasons for the midlife mental health crisis. Subsequently, we translated those into research questions testable with the British birth cohorts. We propose a series of studies using three statistical modelling approaches: descriptive (what is the midlife mental health crisis?), predictive (who is at increased risk of experiencing the midlife mental health crisis?) and explanatory (what are the processes leading to the midlife mental health crisis?).
Keywords
midlife crisis; adult mental health; life course mental health; psychological distress
Introduction
Common mental disorders (including depression and anxiety) are the leading cause of non-fatal disease burden, measured by years lived with disability (
To facilitate further research, we consulted members of the public, mental health professionals and researchers on potential reasons for the midlife mental health crisis. Subsequently, we translated those suggested reasons into research questions that can be tested using the British birth cohorts: the 1946 MRC National Survey of Health and Development (NSHD) (
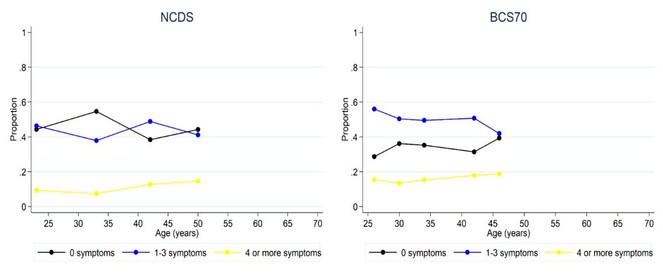
For brevity, we outline recommendations for future research based on the NCDS and the BCS70 due to greater comparability of those two cohorts. These datasets measured mental health (as psychological distress) using the Malaise Inventory (NCDS: at age 23, 33, 42, 44/45, 50; BCS70: at age 26, 30, 34, 42, 46) (
Research agenda
To guide future research on midlife mental health crisis, we propose a series of studies using three statistical modelling approaches: descriptive, predictive and explanatory (
• Descriptive – Study 1
- What is the midlife mental health crisis?
• Predictive – Study 2
- Who is at increased risk of experiencing the midlife mental health crisis?
• Explanatory – Study 3
- What are the processes leading to the midlife mental health crisis?
Describe - what is the midlife mental health crisis?
In descriptive modelling, the focus is on “summarizing or representing the data structure in a compact manner” (
Another step to better understanding the midlife mental health crisis is to investigate how heterogeneous this phenomenon is. Namely, if it is likely to affect the majority of the population—hence shifting the entire distribution towards higher distress—or it is more specific to certain subgroups of the population, for instance to those who have been particularly prone to experiencing mental health problems at earlier ages. The latter can be investigated with finite mixture models, which classify individuals according to their propensity to report psychological distress at ages 23-50 in NCDS and BCS70 (
Identifying potential sub-populations will facilitate the next step in the research agenda—prediction, where characteristics of those experiencing the midlife mental health crisis will be studied. For instance, as seen in Fig.
Likewise, individuals vary greatly in their longitudinal trajectories of psychological distress, which tend to diverge with age—producing a 'fanning out' of psychological distress with age (
Predict – who is at increased risk of experiencing the mental health crisis?
The objective of predictive modelling is prediction of a given outcome, based on the available information (
In this phase, we recommend using outcomes derived through the descriptive step of the research agenda—in addition to summary scores obtained with the Malaise Inventory. These outcomes include cross-sectional latent classes obtained at each studied age (NCDS: at age 23, 33, 42, 44/45, 50; BCS70: at age 26, 30, 34, 42, 46) as well as longitudinal latent profiles modelled across age 33-50. This will help to further understand whether there are any crucial differences in characteristics across subgroups of the population varying in their propensity to experience psychological distress at each studied age and longitudinally. Predictors of the increase in mental health problems between early-30s and 40s/50s may be additionally studied by controlling for psychological distress at preceding age, i.e. at age 33 when psychological distress at age 42 is used as the outcome in the NCDS. After consultation with researchers, mental health professionals and members of public, we identified a list of variables that may be associated with the midlife mental health crisis and can be operationalised by information captured in NCDS and BCS70 (see Table
Key potential reasons for the midlife mental health crisis consistently identified by researchers, mental health professionals and members of public
|
Work factors: high demands, increasing responsibilities, insecurity, uncertainty about progress |
|
Family factors: increased care demands for children and older relatives, role and structural changes |
|
Physical health: decline in physical health, unhealthy behaviours, increased distress |
|
Social factors: loneliness, lack of time for hobbies, social capital |
|
Adverse events: divorce, poor socioeconomic circumstances |
|
Early life factors: general vulnerability to distress (e.g. low cognitive scores, poor child mental health, poor academic achievement, parental death and family characteristics) |
|
Personality and identity (e.g. neuroticism, identity confusion, unmet expectations) |
Explain – what are the processes leading to the midlife mental health crisis?
The final step within the proposed research agenda is to test causal processes leading to the midlife mental health crisis. We suggest selecting variables, from the pool of identified predictors in step 2, which potentially lie on the causal pathway between age (33-36 – 54) and psychological distress and are malleable hence can be targeted by interventions. Estimating the proportion of the effect of age on psychological distress captured by these variables (i.e. mediators), allows for quantifying potential benefits of intervening on these variables (
Conclusion
The proposed research agenda comprises three consecutive steps, where each step addresses an overarching research question in order to increase our understanding of the mental health midlife crisis. We acknowledge that further research questions may arise, for instance, related to differences across the birth cohorts or other potential predictors not yet captured in existing research. However, this agenda provides a comprehensive guide to using existing cohort data as the means to advance our understanding of the midlife mental health crisis—a phenomenon of great importance for public health.
Acknowledgements
The authors would like to thank all the participants of the consultation on reasons for midlife mental health crisis, particularly Professor Marcus Richards and Professor Andrew Oswald. DG was supported by 3+ PhD ESRC funding.
Author contributions
DG and BM conceived, planned and carried out the project. All authors discussed the outcomes of the project, read and contributed to the final manuscript.
Conflicts of interest
The authors declare that they have no conflict of interest.
References
- Life-course and cohort trajectories of mental health in the UK, 1991-2008-A multilevel age-period-cohort analysis.Social Science & Medicine120:21‑30. https://doi.org/10.1016/j.socscimed.2014.09.008
- Is well-being U-shaped over the life cycle?Soc Sci Med66(8):1733‑49. https://doi.org/10.1016/j.socscimed.2008.01.030
- Unhappiness and age. NBER Working Paper No. 26642.National Bureau of Economic Researchhttps://doi.org/10.3386/w26642
- A longitudinal typology of symptoms of depression and anxiety over the life course.Biological Psychiatry62(11):1265‑1271. https://doi.org/10.1016/j.biopsych.2007.05.012
- Healthcare Risk Adjustment and Predictive Modeling.ACTEX Publications
- Cohort profile: 1970 British Birth Cohort (BCS70).International Journal of Epidemiology35(4):836‑43.
- Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015.Lancet388:1545‑602.
- Psychological distress from adolescence to early old age: Evidence from the 1946, 1958 and 1970 British birth cohorts.Psychological Medicine1‑10. https://doi.org/10.1017/S003329172000327X
- Suicides in the UK: 2016 registrations.
- Psychological distress in mid-life: evidence from the 1958 and 1970 British birth cohorts.Psychological Medicine47(2):291‑303. https://doi.org/10.1017/S0033291716002464
- Cohort profile: 1958 British birth cohort (National Child Development Study).Int J Epidemiol35(1):34‑41. https://doi.org/10.1093/ije/dyi183
- Causal Mediation Analysis With Observational Data: Considerations and Illustration Examining Mechanisms Linking Neighborhood Poverty to Adolescent Substance Use.American Journal of Epidemiology188(3):598‑608. https://doi.org/10.1093/aje/kwy248
- Education,undefinedHealth and Behaviour.Longmans,London.
- Age-period-cohort effects on inequalities in psychological distress, 1981-2000.Psychological Medicine32(6):977‑90. URL: https://www.ncbi.nlm.nih.gov/pubmed/12214796
- To Explain or to Predict?Statistical Science25(3):289‑310. https://doi.org/10.1214/10-Sts330
- Age and birth cohort differences in depression in repeated cross-sectional surveys in England: the National Psychiatric Morbidity Surveys, 1993 to 2007.Psychological Medicine42(10):2047‑55. https://doi.org/10.1017/S003329171200013X
- Regression Analysis and Selection via the Lasso.Royal Statistical Society Series58(1):267‑288.
- A Three-way Decomposition of a Total Effect into Direct, Indirect, and Interactive Effects.Epidemiology24(2):224‑232. https://doi.org/10.1097/EDE.0b013e318281a64e
- Cohort Profile: The 1946 National Birth Cohort (MRC National Survey of Health and Development).International Journal of Epidemiology35(1):49‑54.
- Variable selection: current practice in epidemiological studies.European Journal of Epidemiology24(12):733‑736. https://doi.org/10.1007/s10654-009-9411-2
- Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010.Lancet9(382(9904)). https://doi.org/10.1016/S0140-6736(13)61611-6