|
Research Ideas and Outcomes : Grant Proposal
|
|
Corresponding author: Pradeep Joseph (pgj9@scarletmail.rutgers.edu)
Received: 02 May 2018 | Published: 03 May 2018
© 2018 Pradeep Joseph
This is an open access article distributed under the terms of the Creative Commons Attribution License (CC BY 4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Citation: Joseph P (2018) Eliminating disparities and implicit bias in health care delivery by utilizing a hub-and-spoke model. Research Ideas and Outcomes 4: e26370. https://doi.org/10.3897/rio.4.e26370
|
|
Abstract
The state of health disparities in the United States has remained relatively stable over a number of years. Although overall outcomes for all patients have improved, a difference persists in how different racial, ethnic, and gender groups have fared in our health care system. Many programs that have sought to combat this problem have been predicated on the belief that only a small number of providers in the medical community are aware of their own biases. Accordingly, it was believed that bias awareness is the direct conduit for this particular change in the health system. However, the results of such programs have been unsatisfactory. The reason for such ineffectiveness is that many programs have not taken into account the presence of implicit bias within the patient-provider relationship. This complex form of bias operates in specific ways, and must be dealt with appropriately. The use of digital checklists to aid in clinical decision making has proved to be both a way that patients can receive equitable care, and a way to improve overall patient outcomes. Secondly, in order to reach the most at-risk populations, health care must expand beyond the hospital walls, and out into the community. Nurse navigator programs have been shown to accomplish this with great success. Together, checklists and nurse navigators are the necessary next-step in the battle against health care disparities. What’s more, this two-pronged approach is relatively simple to implement. By making use of current electronic medical records, digital checklists can be quickly installed. Likewise, nurse navigator programs, a comparatively inexpensive option, can be rolled out quickly because of their simple design. A focus on the patient-provider relationship and community outreach is critical for progress in eliminating health care disparities.
Keywords
health disparities, implicit bias, clinical checklist, quality of care, health IT, nurse navigator, community health
Introduction
The Problem of Health Care Disparities
Health care providers within the U.S. have sworn allegiance to the principles of justice and egalitarianism from the beginning of their training. Yet, an overwhelming amount of research has indicated that there remains a disparity in today’s health care system among the care different population groups receive. These disparities are most pronounced among different racial and ethnic groups. In a groundbreaking report published by the Institute of Medicine (IOM), black Americans, who are only about 3-6% more likely to deny treatment than other populations, received significantly less needed care than white Americans, even when controlling for factors such as insurance coverage and patient income (
The Failure of Traditional Methods
After the IOM discovered the presence of health care disparities, they offered one solution to this complex problem: raise awareness (
Effects of Traditional Diversity Training in the Workplace: % Change Over Five Years in Representation Among Managers.
Note: n/a indicates no statistical certainty of program's effect.
| Type of Program | White Men | White Women | Black Men | Black Women | Hispanic Men | Hispanic Women | Asian Men | Asian Women |
|---|---|---|---|---|---|---|---|---|
| Mandatory Diversity Training | n/a | n/a | n/a | -9.2 | n/a | n/a | -4.5 | -5.4 |
|
Job Tests |
n/a |
-3.8 |
-10.2 | -9.1 | -6.7 | -8.8 | n/a | -9.3 |
|
Grievance Systems |
n/a | -2.7 | -7.3 | -4.8 | n/a | -4.7 | -11.3 | -4.1 |
Research in psychology has provided a basis for the failure of these traditional programs. One group of researchers took overt measures to minimize bias in one group and compared the facilitatory effect, an indicator of stereotype activation, with that of a control group’s. The results showed that the group exposed to an overt suppression of bias showed an increased, or “rebound,” facilitatory strength (
The Presence of Implicit Bias
One potential reason diversity training programs fail in many different workplace environments is because biases may often be unconsciously held. One study answered the question of why implicit, or unconscious, bias may have a role in the clinical encounter by pointing to the fact that there are not enough black men working within the medical field. In 2012, only about 2% of the graduating medical class in the United States were black men (
Literature Review
Using Digital Checklists for Standardization
One form of bias observed in 2006 at Johns Hopkins Hospital prompted researchers to begin studying ways to reduce treatment disparities. Gender bias was evident from the fact that women were less likely than men to receive intensive treatment for heart attacks, less likely to be sent for knee replacements, and had longer wait times for EKGs (
CDS Checklist Results on VTE Treatment
| Preimplementation (N=1,000) | Postimplementation (N=942) | P-value | |
| Total receiving risk-appropriate VTE prophylaxis | 656 (65.6%) | 849 (90.1%) | <0.0001 |
| Not receiving any form of VTE prophylaxis | 236 (23.6%) | 41 (4.4%) | <0.0001 |
| Total VTE episodes | 25 (2.5%) | 7 (0.7%) | 0.0022 |
| Preventable harm from VTE | 11 (1.1%) | 0 (0) | 0.001 |
| Total 30-day post-discharge VTE | 9 (1.1%) | 2 (0.3%) | 0.0300 |
| Total 90-day post-discharge VTE | 20 (2.7%) | 2 (0.3%) | 0.0003 |
This shows that thousands of patients who arrive at Johns Hopkins Hospital each year at risk for blood clots can receive truly equitable care that does not discriminate based on gender, race, or any other factor (
The Impact of Quality of Care on Health Disparities
In order to measure whether there is a correlation between the improvement in care and the magnitude of health disparities, researchers from Harvard Medical School analyzed quality-of-care data made available from all Medicare managed plans. In 1997, the Centers for Medicare and Medicaid Services (CMS) mandated that all associated managed-care plans publish data relating to the quality of care its patients received. This information is stored in the Health Plan Employer Data and Information Set (HEDIS). The nine clinical parameters chosen as common measures of health care were captured under three headings: breast-cancer screening, diabetes care, and cardiovascular care. For example, under breast-cancer screening, a woman between the ages of 65 and 69 who had not received a mammogram within the past two years would be flagged in the system (
For the two clinical measures in which racial disparities did not improve, control of glycosylated hemoglobin levels and control of LDL cholesterol levels, both under the cardiovascular care heading, there was found to be no statistically significant change. This means that the improvement in care quality has no harmful effects on health disparities. Nevertheless, it is important to recognize that improving the quality of care alone does not accomplish the ultimate goal of eliminating disparities in health care entirely. One point of concern in this study is the lower number of black individuals receiving care. For example, out of those needing care for diabetes, there was a 19.6% reduction in the number of white patients throughout the study, compared with a 31.7% reduction in the number of black patients (
The Nurse Navigator Program
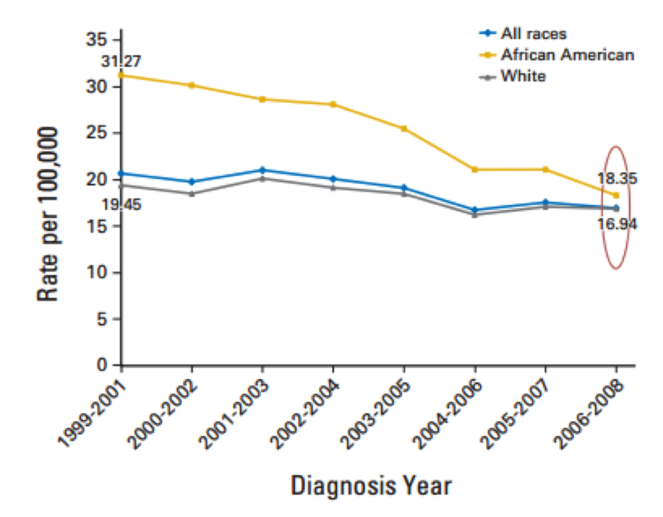
Sending health care workers out into the community as a means to improve a target population’s health is indeed unconventional. However, this is exactly what the state of Delaware accomplished recently by making use of a nurse navigator program. Initially, government officials in Delaware recognized the growing disparity in cancer incidence between its white and black populations. To combat this trend, nurse navigators were hired at each acute care hospital, and were commissioned with specifically reaching African Americans to be screened for colorectal cancer. To that end, they would work with community organizations throughout the state and lead marketing campaigns to reach as many black Americans as possible. Once they agreed to be screened for cancer, the nurse navigators would serve as their primary point of contact. Each patient was assigned a nurse navigator for guidance through the health care system (Fig.
Although a small disparity still exists in colorectal cancer mortality rates, as can be seen in Fig.
Strategy and Plan
Overview
To achieve a meaningful reduction in health care disparities across the United States, I am seeking first to establish a two-year program at two target hospitals. This two-year program will require a 6-month preparation period and will be conducted at the Robert Wood Johnson University Hospital in New Brunswick, NJ, and the University Hospital in Newark, NJ, the two principal teaching hospitals in the Rutgers Health network. Although the two-year time frame poses a limitation for the nurse navigator program, which may require a longer period of time to provide conclusive data, the rate of change over two years can be extrapolated for an eight-year time frame in order to estimate whether this program would produce significantly improved results when compared to the Delaware nurse navigator program. Based on the success of this initiative, steps can be taken to apply similar changes at hospitals nationwide in order to eliminate health disparities. The main features of this program will be the establishment of a hospital-wide CDS checklist, and a nurse navigator program operating out of each hospital. The checklist employed at Johns Hopkins Hospital was developed solely for the Trauma Department in their dealings with patients at risk for blood clots, one common hospital acquired complication. Now, for our target hospitals, checklists for two other hospital acquired complications will be created: hospital acquired infections and pressure ulcers. This way, the efficacy of such checklists for morbidities other than blood clots can be measured. For similar reasons, the nurse navigator program will be expanded to help African American patients receive screenings for breast cancer and cervical cancer, as oppose to colorectal cancer.
Specific Details
The Principal Investigator of this project will be commissioned to oversee the project by managing and coordinating activity between the different organizations that will have to work together in order for the program to be successful. Under these obligations, he or she will be required to hire all of the nurse navigators necessary for the two communities to be reached, and for gathering medical professionals to create the clinical checklist for physicians who deal with patients with the two aforementioned hospital acquired complications. These medical professionals will have each hospital’s institutional review board approves the clinical checklist. The only organization outside of the Rutgers Health network involved in this project will be CTG Health, a health information technology consulting firm, who will be responsible for implementing the digital checklist into the existing electronic health record framework. CTG is a reliable organization because it has accomplished a similar task for the St. Luke’s Health System in Idaho. CTG was able to redesign St. Luke’s online system for patient data and implement new applications, without causing disruptions in workflow (
Budget
Overview
The plans of this proposal is modelled heavily on the success of other programs that have made their associated costs available. Therefore, the budget can be broken down into three simple categories that cover many smaller, and related, expenses Table
Budget Distribution
| Principal Investigator: | $162,220 * 2.5 | $405,550.00 |
| Digital Checklist: | $618,000 * 2 | $1,236,000.00 |
| Nurse Navigator Program: | (2 * ($1.15 * 55,181)) + (2 * ($1.15 * 277,140)) | $764,338.30 |
| Total: | $2,405,888.30 |
Justification
- Principal Investigator: The Principal Investigator will be paid a salary equal to the national average for clinical research directors, $162,220. This salary is multiplied by 2.5 because the project will be in place for 2 years with a 6-month preparation process.
-
Digital Checklist: The checklist implemented at Johns Hopkins Hospital costed a total of $618,000 (
Haut 2014 ). This includes the cost of gathering physicians to develop such checklists, and the implementation of it into the health system as an application by a third-party consulting firm. However, since this project encompasses two different hospitals, $618,000 must be multiplied by 2. -
Nurse Navigator Program: The colorectal cancer screening program in the state of Delaware resulted in an annual cost of $1.15 per resident (
Grubbs et al. 2013 ). This includes the salary for each nurse navigator and the resources they would need to effectively reach their target population. Since this project only involves two communities, we multiply $1.15 by 55,181 and 277,140, the number of residents in New Brunswick and Newark, respectively. Also, because this is a two-year program, we must multiply each value by 2 and add up the costs for New Brunswick and Newark in order to estimate how much a nurse navigator system will cost overall.
Discussion
At this time in American history, a tipping point has been reached where the health disparities between different populations must be accounted for. Methods that have primarily focused on making clinicians more aware of their own biases have backfired. From previous research, it is clear that redesigning how physicians interact with patients by introducing a clinical checklist greatly increases the quality of care. Furthermore, this standardized quality of care has been shown to lead to significant reductions in health care disparities. However, changes within the walls of the hospital are not enough to completely eliminate inequalities. There must be an outreach into the community by care coordinators to ensure that at-risk populations are receiving an appropriate level of care. The hub-and-spoke design of this proposal seeks to accomplish this task. When the final data from this project is obtained, the Principal Investigator will analyze it and make a public report for leaders in the field to determine the program's merit as a new health care delivery paradigm. This hub-and-spoke model shows great promise for achieving a health care delivery system that is free of disparities.
References
-
Bias, black lives, and academic medicine.The New England Journal of Medicine372:1087‑1089. https://doi.org/10.1056/NEJMp1500832
-
Unconscious (implicit) bias and health disparities: Where do we go from here?The Permanente Journal15:71‑78.
-
St. Luke’s Health System Relies on CTG for Implementation Leadership. https://www.ctg.com/fr/case-study/st-lukes-health-system-relies-ctg-implementation-leadership. Accessed on: 2017-4-12.
-
Diversity management in corporate America.Harvard Business Review6(4):21‑27. https://doi.org/10.1525/ctx.2007.6.4.21
-
Why Diversity Programs Fail. https://hbr.org/2016/07/why-diversity-programs-fail. Accessed on: 2017-4-22.
-
African American health disparities compared to non-hispanic whites. http://familiesusa.org/product/african-american-health-disparities-compared-to-non-hispanic-whites. Accessed on: 2017-4-17.
-
Eliminating racial disparities in colorectal cancer in the real World: It took a village.Journal of Clinical Oncology31:1928‑1930. https://doi.org/10.1200/JCO.2012.47.8412
-
Summaries of Independent Scientist (K) Awards. Agency for Healthcare Research and Quality. https://www.ahrq.gov/funding/training-grants/grants/active/kawards/Kawdsumhaut.html. Accessed on: 2017-4-04.
-
Estimating the economic burden of racial health inequalities in the United States.International Journal of Health Services41:231‑238. https://doi.org/10.2190/HS.41.2.c
-
Out of mind but back in sight: Stereotypes on the rebound.Journal of Personality and Social Psychology67:808‑817. https://doi.org/10.1037/0022-3514.67.5.808
-
A fix for gender bias in health care? Check. https://www.nytimes.com/2017/01/11/opinion/a-fix-for-gender-bias-in-health-care-check.html?_r=0. Accessed on: 2017-3-03.
-
Unequal treatment: Confronting racial and ethnic disparities in health care.National Academies Press.
-
Trends in the quality of care and racial disparities in medicare managed care.The New England Journal of Medicine353:692‑700. https://doi.org/10.1056/NEJMsa051207
-
Judgment under uncertainty: Heuristics and biases.Science185:1124‑1131. https://doi.org/10.1126/science.185.4157.1124
-
Impact of venous thromboembolism prophylaxis “smart order set”: Improved compliance, fewer events.American Journal of Hematology88:545‑549. https://doi.org/10.1002/ajh.23450